Microscopic colitis
Collagenous and
lymphocytic colitis
The informed patient

6th updated and
revised edition 2020
Publisher
©
2020 Dr. Falk Pharma GmbH
All rights reserved.

Prof. Dr. Andreas Tromm, Hattingen (Germany)
The informed patient
Microscopic colitis
Collagenous and
lymphocytic colitis

Microscopic colitis – Collagenous and lymphocytic colitis
Address of the author
Prof. Dr. Andreas Tromm
Klinik für Innere Medizin
Augusta-Kranken-Anstalt gGmbH
Betriebsstelle EVK Hattingen
Akademisches Lehrkrankenhaus
der Universität Duisburg-Essen
Bredenscheider Str. 54
45525 Hattingen
Germany
www.klinik-gastroenterologie.de
3
Introduction 4
Clinical presentation 6
Causes and development of
microscopic colitis 9
Diagnosis 11
Treatment 14
Frequently asked questions
about microscopic colitis 17
Contents
4
Microscopic colitis – Collagenous and lymphocytic colitis
Introduction
The term microscopic colitis encompasses two different
disorders of the colon known as collagenous colitis and
lymphocytic colitis.
Both disorders are characterized by non-bloody watery
diarrhea and are sometimes referred to as watery diar-
rhea syndromes (Fig. 1).
Microscopic
colitis
Watery diarrhea
syndrome
Fig. 1: Definition of microscopic colitis.
Collagenous colitis Lymphocytic colitis

5
The term microscopic colitis describes a chronic in-
flammatory disease of the colon (“colitis” comes from
the Latin term “colon” and the ending “-itis”, which is
used in medicine to refer to inflammation) that a doctor
cannot identify by colonoscopy with the naked eye
because the mucosa of the colon appears normal. In
order for the disease to be diagnosed, the doctor must
therefore remove a small tissue sample and examine
it under a microscope. This is the only way to diagnose
microscopic colitis.
For collagenous colitis, a thickened collagen layer
becomes visible when the tissue samples are stained
using special methods, whereas lymphocytic colitis
is detected as an increased number of a specific type
of white blood cells called lymphocytes (see page 12).
Our understanding of microscopic colitis has expand-
ed greatly since it was first described in the 1970s.
Because the disease is so difficult to diagnose, it is not
well known, even though it is thought to occur about
as often as the inflammatory bowel diseases of Crohn’s
disease and ulcerative colitis. The number of undiag-
nosed cases is likely high.
The standard of care is budesonide (taken orally as
capsules or granules), a locally-acting corticosteroid
drug that inhibits inflammation in the gut. Depending
on the form of microscopic colitis, budesonide can
be used to treat the symptoms of acute disease or in
case of chronic disease it can also be used to prevent
the recurrence of diarrhea.
Introduction
6
Microscopic colitis – Collagenous and lymphocytic colitis
Clinical presentation
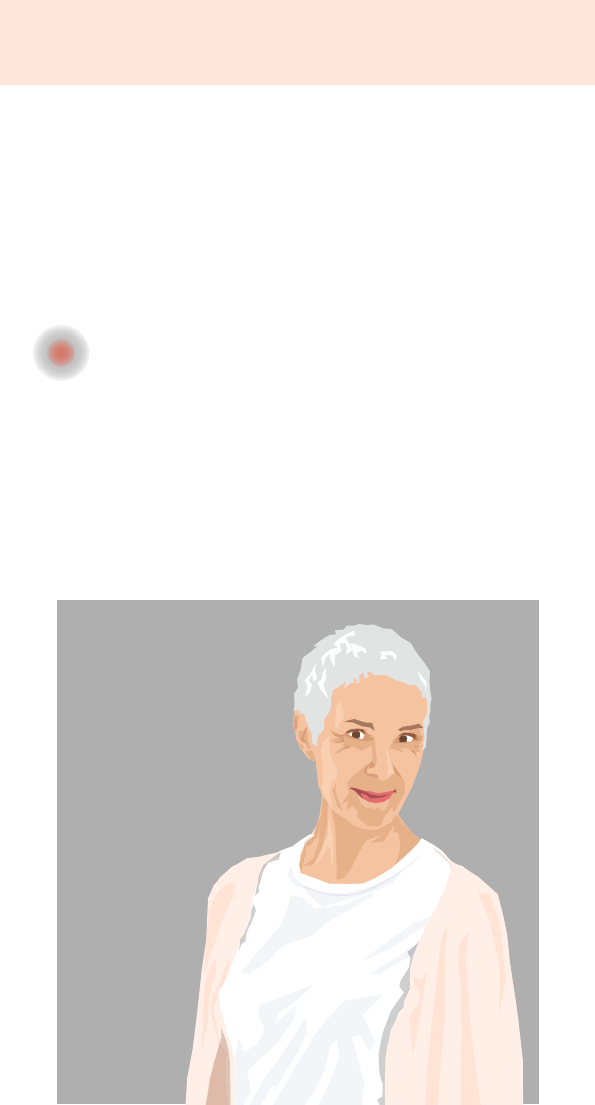
Microscopic colitis primarily affects older women.
The defining symptom of microscopic colitis is watery
diarrhea, which can occur suddenly and may mimic
an infection. A large study in Sweden also reported
the following symptoms:
• In almost 30% of patients: nocturnal diarrhea
• In over 40% of patients: weight loss
• In over 40% of patients: abdominal pain
• In over 20% of patients: nausea
• In over 10% of patients: flatulence
Although the precise
cause of weight loss
remains unclear, it appears
likely that patients eat
fewer calories due to
well-intentioned dietary
restrictions which cause
them to lose weight.
Patients rarely have issues
with dehydration despite
the frequent diarrhea.
Fecal incontinence and fatigue are
other symptoms that occur with microscopic colitis
and greatly impair patients’ quality of life.
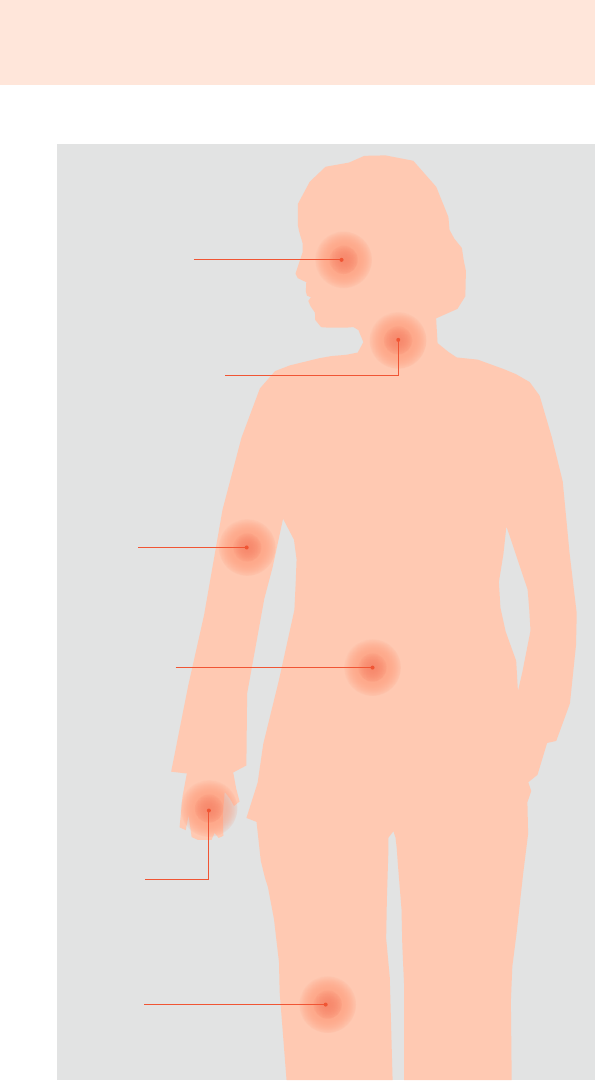
30–50% of patients with microscopic colitis may also
experience symptoms or conditions in other organs
outside of the gut, for example rheumatoid arthritis
of the joints, psoriasis of the skin, or even thyroid gland
dysfunction (Fig. 2). These issues require additional
treatment.
7
Fig. 2: Conditions that may accompany microscopic colitis.
Clinical presentation
Mucosal dryness
Thyroid dysfunction
Psoriasis
Perfusion
disorders
Celiac disease
Joint pain

8
Microscopic colitis – Collagenous and lymphocytic colitis
Several studies have shown that patients with micro-
scopic colitis also frequently have celiac disease
(or gluten intolerance) and vice versa.
Therefore, patients should be checked for both condi-
tions. A recent study reported that 12.9% of patients
with collagenous colitis also have celiac disease.
Microscopic colitis generally has a benign outcome,
although about 40% of patients complain of chronic
(meaning permanent or continuously recurring) watery
diarrhea. However, this diarrhea does not increase the
risk of developing colorectal cancer.
In order to diagnose the condition, doctors must rule
out the possibility of other conditions with similar symp-
toms: Typical gut disorders associated with diarrhea but
not with weight loss include irritable bowel syndrome
(diarrhea-type) and intolerance to several different types
of foods, such as the very common lactose intolerance.
Microscopic colitis can usually be clearly distinguished
from Crohn’s disease and ulcerative colitis (together
known as inflammatory bowel disease), since a colo-
noscopy reveals a typical pattern of intestinal mucosa
pathology with ulcers in inflammatory bowel disease.
When inflammatory bowel disease spreads to the
colon, as is often the case, diarrhea is usually bloody.
9
Causes and development
of microscopic colitis
Although the exact causes of microscopic colitis remain
unknown, several theories have been proposed.
Several studies have proposed that microscopic colitis
may be caused by the increased use of certain medi-
cations, typically those used to manage joint pain.
These include drugs called “non-steroidal anti-inflam-
matory drugs” as well as drugs used to treat high
cholesterol levels or to stop blood clotting.
Case reports have suggested that proton-pump in-
hibitors may play a role in the development of micro-
scopic colitis, but this link has not been thoroughly
investigated.
A retrospective study showed
that the percentage of
smokers is higher among
collagenous colitis patients
than among the population
as a whole. This study was
the first
to demonstrate
a potential
effect of nico-
tine on the development of
microscopic colitis. This effect
might be based on the fact that nicotine increases
the permeability of the intestinal mucosa. Continued
nicotine consumption also reduces a patient’s response
to budesonide treatment.
It is theoretically possible that increasing the permeability
of the intestinal mucosa (the cause of which remains
unknown) may allow digested food to migrate into
the intestinal wall and disrupt the function of the gut.
A recent study reported that the microbial flora of
the gut has a different composition in patients with
microscopic colitis than in healthy controls.
Causes and development of microscopic colitis

10
Microscopic colitis – Collagenous and lymphocytic colitis
Antibodies targeting parts of the body itself have been
detected in about half of all patients with lymphocytic
colitis. These antibodies are directed at the gut, and as
a result this disease might need to be classified as an
“autoimmune disorder”.
In contrast, antibodies are frequently found in collagen-
ous colitis patients that target bacteria – bacteria which
themselves cannot be detected in the body. This may
be a sign of a prior infection by these bacteria. Alter-
natively, it might reflect the increased permeability of
the intestinal wall, which could lead to the production
of antibodies against microbes located in the wall
(e.g. Yersinia species).
It is still unknown how these phenomena result in a
thickening of the collagen layer in collagenous colitis or
lead to an accumulation of immune cells (lymphocytes)
in the intestinal mucosa in lymphocytic colitis.
However, we do know that the collagen deposits found
in collagenous colitis patients do not result from the
overproduction of collagen, but rather from reduced
degradation of collagen.
Interestingly, in patients with an artificial outlet to the
gut, known as a stoma, the collagen layer in the gut
segments downstream of the stoma returns completely
to
normal, resulting in a cure of the disease. This suggests
that the contents of the gut are important for develop-
ing the disease.
11
Diagnosis
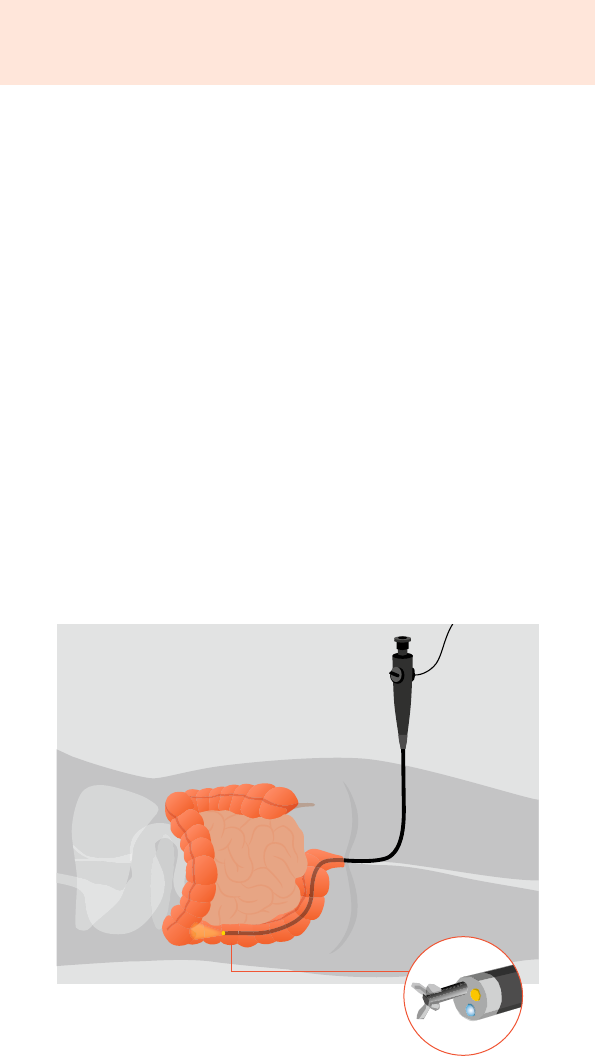
In order to confirm the diagnosis of microscopic colitis,
experience has shown that patients with watery diarrhea
lasting longer than 4 weeks should be examined by co-
lonoscopy. If the results of the colonoscopy are normal,
meaning the doctor cannot detect any changes to the
mucosa with the naked eye, small tissue samples should
be collected from the intestinal mucosa (using biopsy
forceps) (Fig. 3). The diagnosis is based on an assessment
of this samples under the microscope. About 10%
of patients with watery diarrhea lasting longer than
4 weeks and normal colonoscopy results are diag-
nosed with microscopic colitis. It is important to collect
samples from different segments of the colon in all
patients, since collagenous colitis is limited only to the
ascending segment of the colon in about one-quarter
of patients, to give one example.
Diagnosis
Fig. 3: Colonoscopy with collection of
tissue samples from different segments
of the colon.
Biopsy forceps,
approx. 3 mm
12
Microscopic colitis – Collagenous and lymphocytic colitis
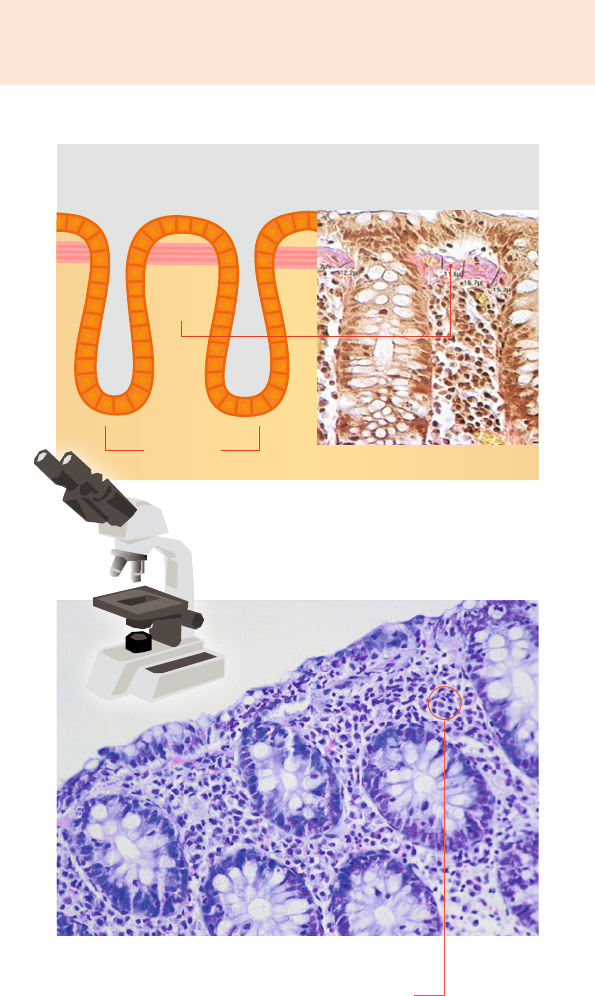
Collagen
layer
Epithelium
Surface of the intestinal mucosa
–10 µm
Crypts
Fig. 4a: Diagram (left) and microscopic image
(right) of the intestinal mucosa in a patient with
collagenous colitis. The thickened collagen
layer, which is stained pink, is clearly visible.
Fig. 4b: Microscopic image of the intestinal mucosa
in a patient with lymphocytic colitis showing
accumulation of lymphocytes (small purple dots).

13
When intestinal tissue samples are examined under the
microscope, both disorders are characterized by very
typical findings: Using specific staining methods, a
thickened collagen layer (pink) is visible in the intestinal
mucosa in patients with collagenous colitis (Fig. 4a).
Collagen fibers are a specific protein structure in the
body that helps support tissues. While this collagen
layer is less than 5 micrometers (one-millionth of a
meter) wide in healthy people, it is at least 10 micro-
meters wide in collagenous colitis patients and is easily
visible under the microscope after staining.
For people with lymphocytic colitis, doctors find an
increased accumulation of immune cells (lymphocytes,
a subgroup of white blood cells) in the tissue samples.
The lymphocyte count is about 4- to 5-fold higher
than in healthy people (Fig. 4b).
However, it is still not known what effect the thickened
collagen layer or the increased accumulation of inflam-
matory cells has on the course of the disease.
It is currently not possible to diagnose these diseases
by blood test. Levels of calprotectin, which is a marker
of inflammation, may be elevated. However, this finding
is not specific and does not prove somebody has micro-
s
copic colitis. On the other hand, it does mean that
patients with persistent diarrhea and elevated calpro-
tectin levels should always be referred to a colonoscopy
for diagnostic purposes.
Diagnosis

14
Microscopic colitis – Collagenous and lymphocytic colitis
Treatment
The goal of treatment is to improve or completely
eliminate the symptoms of the disease, which improves
patients’ quality of life.
Budesonide
Drug treatment using the active substance budesonide
is the standard treatment option and is the treatment
which has been tested the most in controlled studies.
Budesonide is a modern corticosteroid drug that has
very good local anti-inflammatory effects on the
intestinal mucosa.
The substance was originally used as a spray to treat
asthma. It has also been used to treat inflammatory
bowel disease since the 1990s. Budesonide, which is
given as granules or in a capsule, is not released until
it reaches the border between the small intestine and
the ascending colon thanks to a special manufacturing
process. Once it arrives in the ascending colon, it has
potent local anti-inflammatory effects on the mucosa
that are stronger than the effects of classical corticoster-
oids. The special benefit of budesonide is the fact that
over 90% of it is directly metabolized by the liver after
being active in the gut. As a result, only a small percent-
age of the drug circulates in the bloodstream, leading
to many fewer steroid-like side effects compared with
classical corticosteroid drugs. Budesonide is thus an
optimal choice for achieving a high degree
of local effectiveness at the intestinal
mucosa while keeping the rate of
side effects low.
Budesonide is generally taken
at a dose of 9 mg per day for
8 weeks for the treatment of acute
disease. In clinical studies, this treatment
was associated with clinical improvement
and absence of diarrhea in about 80% of patients.

15
However, patients often experience a recurrence of
the disease 2 months after stopping the drug. If this
occurs, treatment may be resumed at a reduced dose
of 4.5–6 mg budesonide per day. The doctor and
the patient will need to discuss the precise length of
treatment. Studies have shown that this treatment
reduces the probability that symptoms will return
within 6–12 months by about 60% in patients with
collagenous colitis.
Prednisolone
The classical corticosteroid prednisolone was frequently
used in the past to treat patients with microscopic
colitis. However, in contrast to budesonide, predniso-
lone is initially absorbed into the bloodstream after
being ingested. As a result, it not only provides the
desired therapeutic effect but also frequently leads to
severe forms of the typical side effects of steroid drugs.
These include “moon face” (a rounding of the face),
abdominal obesity, high blood pressure, mental health
disorders, and weakening of the immune system.
Bismuth
This drug has antibiotic and anti-inflammatory proper-
ties and is included in some combination drug treat-
ment regimens when budesonide does not improve the
symptoms of disease or is not tolerated by the patient.
However, very few clinical studies have been performed
on bismuth. Furthermore, bismuth products should
not be taken for longer than 8 weeks since they may
accumulate in the body.
Other treatment options
Several open-label (i.e. non-controlled) studies and case
reports have investigated the effects of the probiotic
(bacteria that have a beneficial or potentially beneficial
effect on the gut) E. coli Nissle 1917 and of immuno-
suppressants (azathioprine, methotrexate, and different
antibodies targeting inflammatory factors). Immuno-
suppressant therapy should be taken into consideration
Treatment

16
Microscopic colitis – Collagenous and lymphocytic colitis
for patients who do not respond to standard treatment
with budesonide.
Loperamide, a drug that can stop acute diarrhea by
inhibiting bowel motility, is also sometimes used for
short-term symptom relief. However, it does not treat
the actual cause of diarrhea, which is inflammation
of the intestinal mucosa. Loperamide should be taken
as briefly periods as possible and only after consulting
a doctor.
Other treatment options, such as incense extract,
cholestyramine, or mesalazine, have either not been
adequately studied at present or did not bring about
the desired treatment outcome. Therefore, these drugs
should only be taken as part of any future clinical
studies.
17
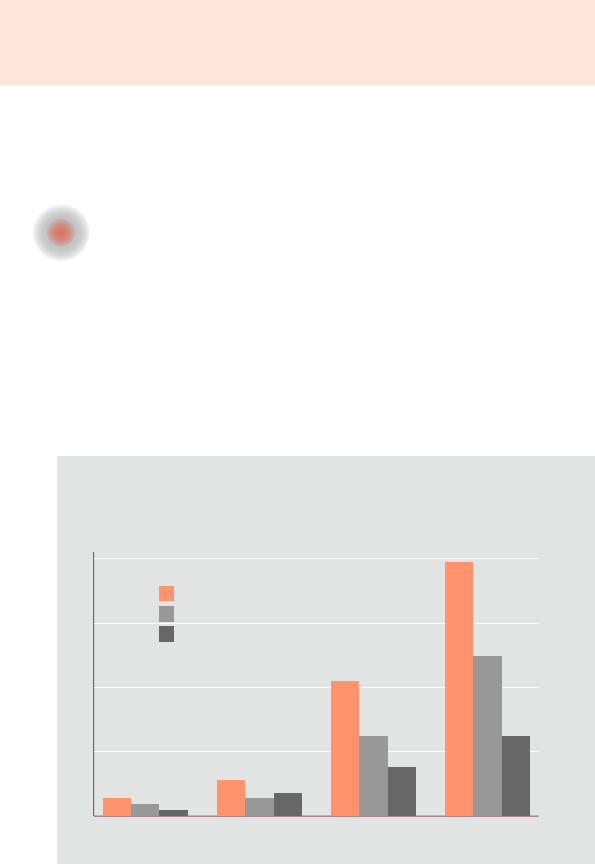
1985–89 1990–93 1994–97 1998–2001
20
15
10
5
0
Microscopic colitis
Lymphocytic colitis
Collagenous colitis
Frequently asked questions about
microscopic colitis
? How common is microscopic colitis?
According to the most recent statistics (including those
from the US), microscopic colitis is being diagnosed
with increasing frequency (Fig. 5). This increase is likely
due to both improvements in diagnosis as well as a
real increase in the number of actual cases. The figures
reveal an annual incidence (rate of new cases) of about
20 patients per 100,000 inhabitants.
Cases per 100,000 inhabitants
The annual incidence of collagenous colitis varies
greatly from one country to the next, for example
at 1–2 cases per 100,000 inhabitants in Spain versus
16 new cases per 100,000 inhabitants in Denmark.
Frequently asked questions about microscopic colitis
Fig. 5: Overview of the incidence of lymphocytic and collagenous
colitis (from a survey in the US).
18
Microscopic colitis – Collagenous and lymphocytic colitis
Little data is available on lymphocytic colitis. The rate
of new cases in Scandinavia is thought to be 4 per
100,000 inhabitants.
Epidemiological studies from the US and Denmark both
report an increase in the rates of new cases in both
countries (over the past several years).
? Are there any factors that increase
the chances of microscopic colitis?
All of the studies conducted to date show that women
develop microscopic colitis about 5 times as often
as men. The risk increases even more greatly among
women above the age of 65. This is true for both
collagenous and lymphocytic colitis. The reasons for
this trend are not known.

19
In addition, patients already suffering from certain
diseases of the immune system (called autoimmune
disorders) appear to develop microscopic colitis more
often than patients without pre-existing autoimmune
disorders. This includes patients with hypothyroidism
and celiac disease. Up to 40% of all patients with
microscopic colitis also suffer from an autoimmune
disorder.
Patients with microscopic colitis are more likely to have
celiac disease and vice versa; therefore, patients with
one of these conditions should be tested for the other
(by transglutaminase antibodies or duodenal biopsy).
About 10% of patients also report a history of cancer.
The majority of these cases involve colorectal cancer,
breast cancer, prostate cancer, or lung cancer. Cancer
patients are at a higher risk of developing microscopic
colitis than the general population, especially women
over the age of 65.
Patients with diabetes may also potentially be at a higher
risk of microscopic colitis. This appears to be the case
primarily for older men.
Overall, more research is needed to investigate a poten-
tial link between microscopic colitis and the disorders
listed here, as well as their underlying causes.
Frequently asked questions about microscopic colitis
20
Microscopic colitis – Collagenous and lymphocytic colitis
? What is known about the causes of
microscopic colitis?
The ultimate cause of microscopic colitis remains
unknown.
It is notable that increased use of pain medicines
(including ibuprofen and acetylsalicylic acid) has been
identified as a potential trigger in a relevant number
of patients. These medicines may increase the perme-
ability of the intestinal mucosa, which might promote
the absorption of other substances that trigger the
disease which are not yet known. However, other
drugs, such as simvastatin (used to lower cholesterol),
ticlopidine (used to reduce blood clotting), or acarbose
(used to treat diabetes), have also been reported to be
potential triggers of microscopic colitis. The potential
role of proton-pump inhibitors has not been conclusive-
ly determined.
Studies have also shown that the percentage of colla-
genous colitis patients who are smokers is significantly
higher than in the population as a whole. Smoking
should therefore be avoided since nicotine increases the
permeability of the intestinal wall. Continued nicotine
consumption also lowers a patient’s response to bude-
sonide treatment.
Several different studies have detected antibodies to
Yersinia in about 80% of patients. Yersinia are bacteria
that can lead to an infection of the intestinal mucosa.
In contrast, Yersinia are only rarely detected in the stool
of microscopic colitis patients.
These findings can be interpreted as a reflection of the
increased permeability of the intestinal wall for Yersinia
leading to secondary antibody production.
There is also evidence that microscopic colitis occurs
more frequently within families. However, it remains
unclear whether this points to a genetic component.
21
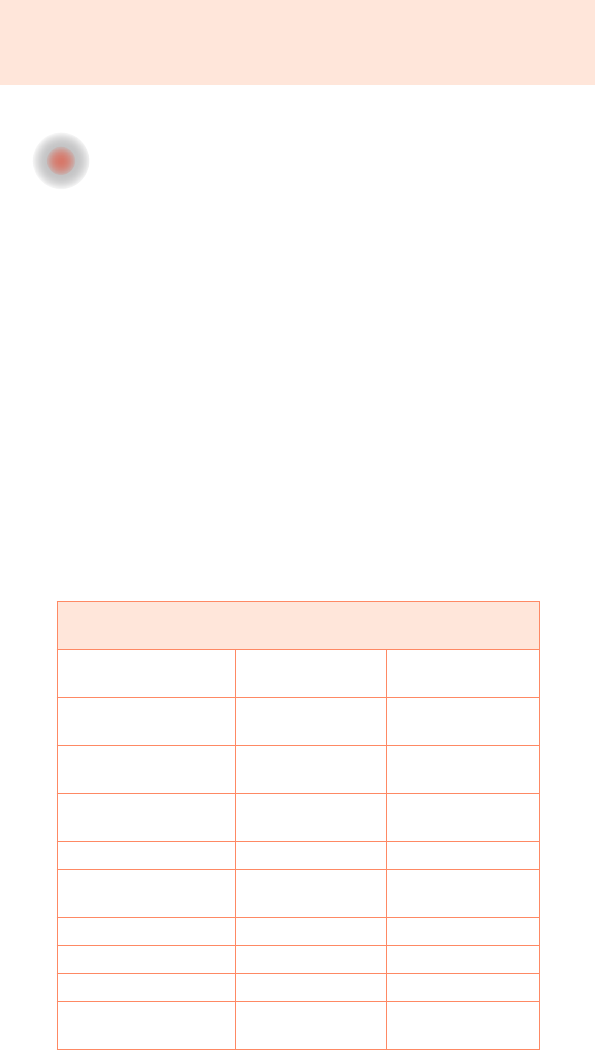
? How does microscopic colitis differ
from irritable bowel syndrome?
The primary symptom of both microscopic colitis and
irritable bowel syndrome is chronic, non-bloody, usually
watery diarrhea.
Endoscopy findings and stool tests for microbes are
typically normal in both diseases. Collection and micro-
scopic examination of tissue samples is thus important
for the diagnosis of both. These examinations clearly
reveal the characteristic signs of microscopic colitis and
allow it to be confidently differentiated from irritable
bowel syndrome.
There are also other characteristics (see Table 1) that
tend to point to one or the other condition. These
characteristics may help confirm, yet cannot replace,
a microscopic diagnosis.
Primary symptoms of irritable bowel syndrome –
Microscopic colitis
Irritable bowel
syndrome
Microscopic
colitis
Initial onset of disease
often below age 50
women ≥ men
often above age 50
women >> men
Stool consistency soft – variable –
firm
watery/soft
Abdominal pain/
discomfort
obligatory variable
Nocturnal diarrhea very rare possible
Sensation of in-
complete evacuation
common no
Weight loss rare common
Fecal incontinence rare common
Bloating common rare
Autoimmune
comorbidities
no yes
Frequently asked questions about microscopic colitis
Table 1

22
Microscopic colitis – Collagenous and lymphocytic colitis
? What is the explanation for the thickening of
the collagen layer in the intestinal mucosa?
The increase in the size of the collagen layer in
collagenous colitis is not due to increased collagen
production but rather to decreased collagen degra-
dation. However, the precise mechanisms leading to
this reduced degradation of collagen in the intestinal
mucosa have not been studied in depth. It is also not
known whether and how thickening of the collagen
layer triggers the typical symptoms of collagenous
colitis.
? Are there any signs of microscopic colitis
outside of the gut?
Microscopic colitis may be accompanied by a number
of other different conditions that indicate a reaction
by the immune system to the tissues of the body. These
include rheumatic joint pain, psoriasis, celiac disease,
thyroid dysfunction, perfusion disorders, and mucosal
dryness (see also Fig. 2).
? Is a proctoscopy sufficient for diagnosis?
Because microscopic colitis most frequently affects
the ascending segment of the colon, a proctoscopy is
not sufficient for diagnosis. The entire colon should
be examined in every patient together with collection
of tissue samples from the different segments of the
colon. If this is not performed, up to 40% of patients
with microscopic colitis may be missed.

23
? Does microscopic colitis increase the risk
of colorectal cancer?
No. There are no indications that polyps or colorectal
cancer develop more often in patients with collagenous
or lymphocytic colitis. In general, the diagnosis of
microscopic colitis has a favorable prognosis, and the
symptoms can be managed well with the drug
budesonide.
? Are there any concerns about pregnancy?
No. There are no concerns about pregnancy with
regard to the disease itself. However, each drug taken
should be reviewed to make sure there are no restric-
tions on its use during pregnancy or while breast-
feeding. In any case, the disease tends to afflict older
patients who have already gone through menopause.
? Are there any dietary factors that have
a positive effect on microscopic colitis?
There are no confirmed results about any potential
effects of dietary factors that might trigger these
diseases. It also remains unknown whether adding or
removing specific foods from one’s diet may have a
positive or negative effect on the course of the disease.
However, because the primary symptom
of the disease is watery diarrhea, lactose
intolerance and celiac disease should
be ruled out as potential causes
during the pre-diagnosis phase.
For both of these disorders, there is
a clear recommendation to maintain
a lactose-free or gluten-free diet.
Frequently asked questions about microscopic colitis
24
Microscopic colitis – Collagenous and lymphocytic colitis
Studies have shown that fasting can lead to a major
improvement in the diarrheal symptoms of collagenous
colitis. However, prolonged fasting does not represent
a long-term treatment option for microscopic colitis.
? Can surgery help microscopic colitis?
In the past, surgery has only been performed for very
severe cases of microscopic colitis, which are very rare.
However, the results from these patients have shown
that when patients have an artificial intestinal opening
(stoma) to empty their digestive tract, both the inflam-
mation and the thickened collagen layer heal in the
downstream segment of the gastrointestinal tract that
is now absent of stool. This fact suggests that certain
factors in the contents of the gut may be important
triggers of microscopic colitis.
? Is the disease ever improved or cured
by itself?
Studies on the long-term progression of collagenous
colitis have shown that some patients remain symptom-
free for a long time after a successful first round of
treatment and have no need for any further medications
.
In one of these studies, 23% of patients still had
no watery diarrhea after 10 years. On the other hand,
symptoms returned in two-thirds of patients within
2 months of stopping treatment. If this happens, a new
round of treatment or a low-dose maintenance therapy
is recommended both for patients with collagenous
colitis and with lymphocytic colitis.
25
? Can binding or bulking agents have a positive
effect on diarrhea?
In cases of mild diarrhea, taking bulking agents or bile
acid sequestrants is often sufficient to increase the
consistency of stool and reduce the frequency of bowel
movements. In one small study, diarrhea resolved in
over 20% of patients taking a bulking agent (such as
psyllium husk).
? How long should budesonide be taken
during the acute phase of the disease?
In the treatment studies that have been performed on
budesonide to date, the drug was given at a dose of
9 mg per day over a period of 6 or 8 weeks. The majority
of patients were nearly completely free of symptoms
within 14 days of starting this treatment plan.
Budesonide is taken as a single dose in the morning.
? Is there a maintenance therapy for
microscopic colitis?
After finishing budesonide therapy for the treatment
of acute microscopic colitis, patients frequently start to
experience diarrhea again within the first 2 months and
thus require further treatment. Several placebo-controlled
studies have all shown that, after achieving clinical
improvement for acute disease with 9 mg budesonide,
continuing treatment with 4.5–6 mg budesonide per
day for 6–12 months can lead to a significant reduction
in the rate of recurrence.
Frequently asked questions about microscopic colitis
26
Microscopic colitis – Collagenous and lymphocytic colitis
Notes
27


BU82E 6-8/2020 POP
