INFORMATION SHEET
MICROSCOPIC COLITIS
1
Crohn’s & Colitis UK | www.crohnsandcolitis.org.uk
INTRODUCTION
Microscopic Colitis is an Inammatory Bowel Disease (IBD) that affects the large
bowel (colon and rectum). It isn’t always as well-recognised as Crohn’s Disease or
Ulcerative Colitis, other forms of IBD.
It can take to time to get a diagnosis of Microscopic Colitis. And dealing with
watery poo, tummy cramps, and rushing to the toilet can all be hard to manage.
But you’re not alone; we’re here to support you. Many people respond well to
treatment and often symptoms go away when you nd what’s right for you.
If you’ve just been diagnosed or want to know more about Microscopic Colitis, this
information is for you.
WHAT IS MICROSCOPIC COLITIS
Microscopic Colitis affects the part of the gut known as the large bowel – the colon
and rectum. The large bowel, or colon’s main job is to absorb water from your poo,
so you can pass a solid but soft and well-formed poo.
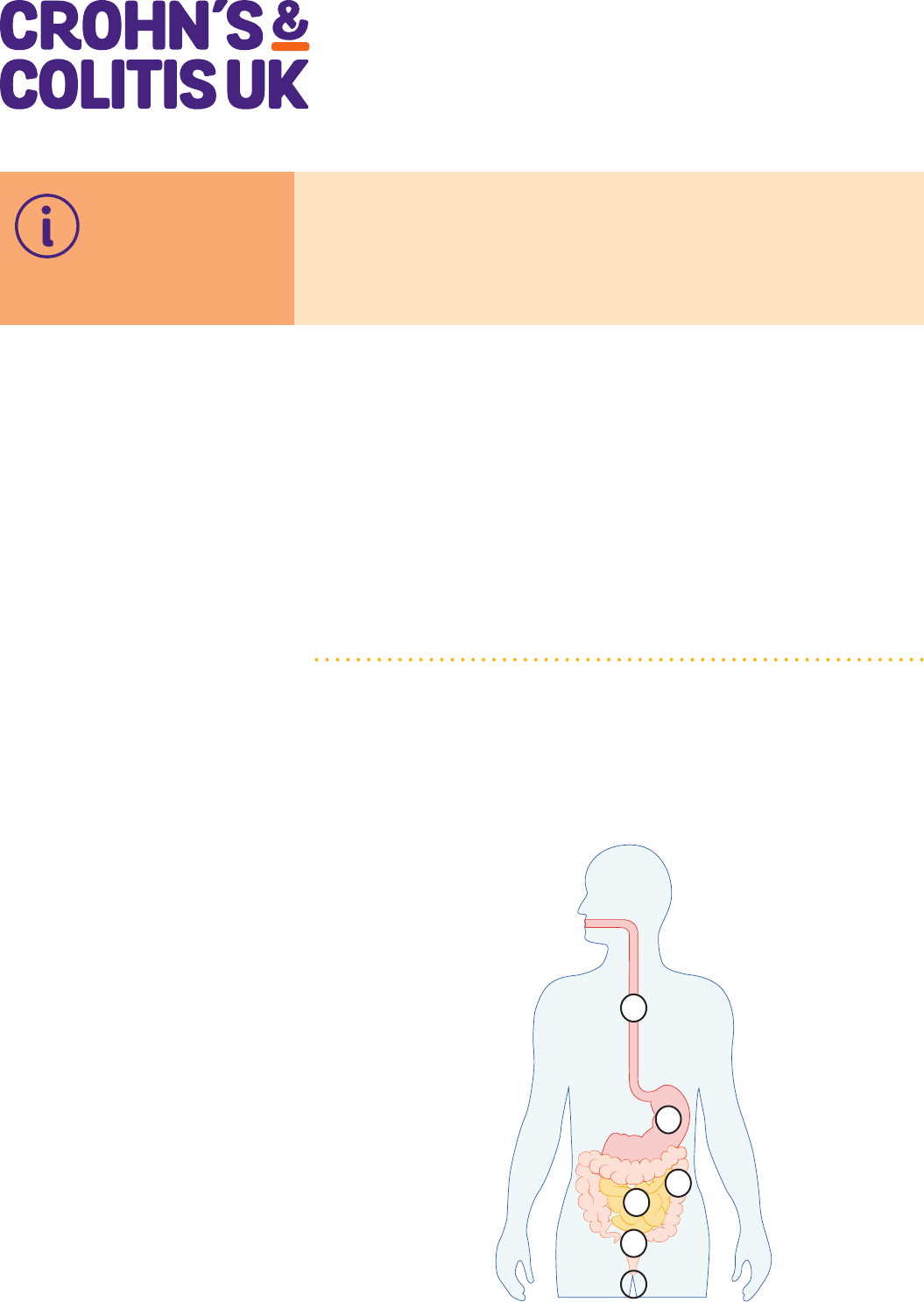
THE GUT
2
1 OESOPHAGUS
2 STOMACH
3 SMALL BOWEL
4 COLON
LARGE BOWEL
5 RECTUM
6 ANUS
3
4
5
}
6
2
1
MICROSCOPIC COLITIS
2
Crohn’s & Colitis UK | www.crohnsandcolitis.org.uk
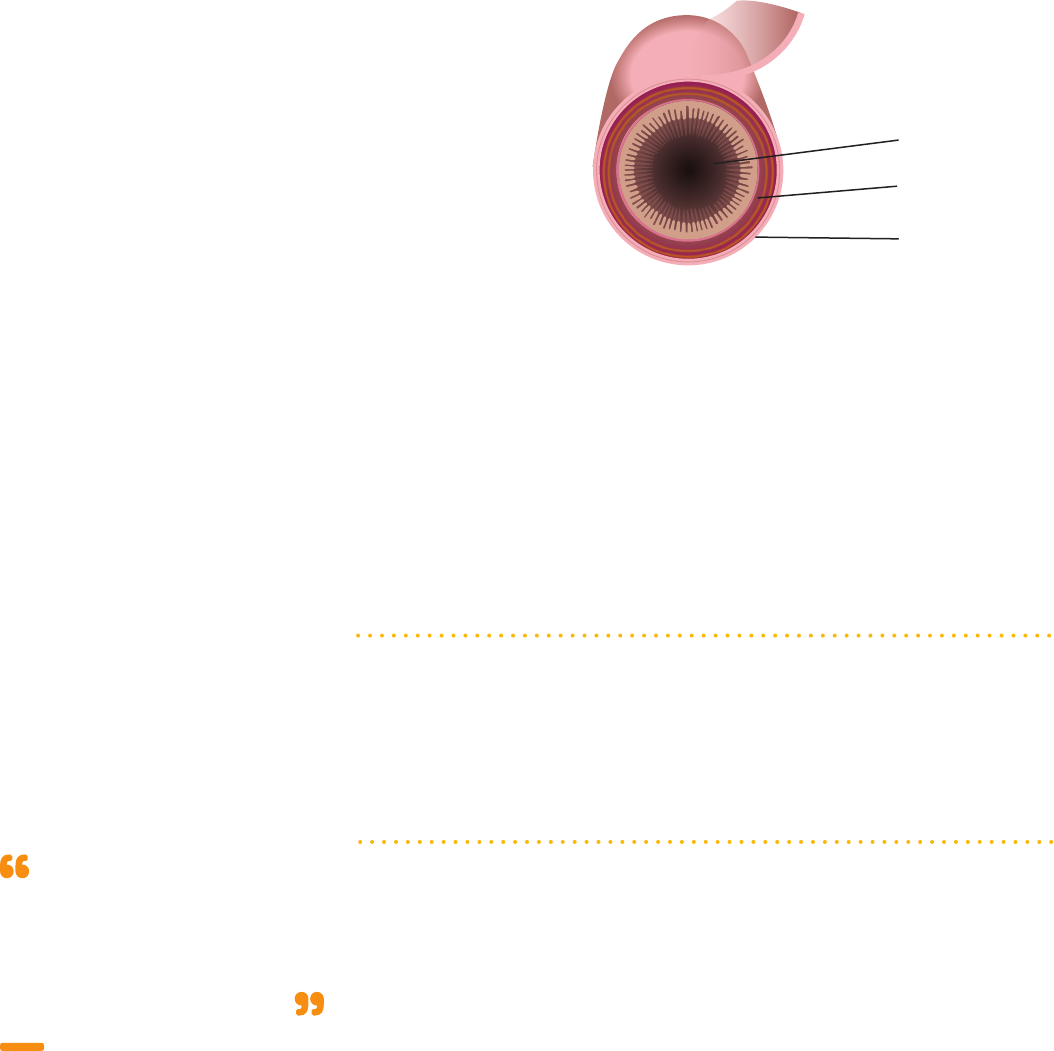
The walls of your bowel have layers. In Microscopic Colitis the inner lining becomes
inamed. But this change can only be seen when a sample of tissue (biopsy) is
taken from your colon and looked at under a microscope.
BOWEL LAYERS
INNER LINING
MIDDLE LAYER
OUTER LAYER
There are two types of Microscopic Colitis:
• Lymphocytic Colitis (LC) – where the inner lining has more white blood cells
(lymphocytes) than usual.
• Collagenous Colitis (CC) – where the inner lining has a thicker layer of collagen,
a protein important in providing structure in the body, than usual. There may also
be more white blood cells present.
Microscopic Colitis is the umbrella term for both LC and CC. Although they look
different under the microscope, symptoms and treatment are the same. However
slightly more people have LC, and women are more likely to have CC. Some people
may even have both types of Microscopic Colitis, but at different times.
HOW MICROSCOPIC COLITIS AFFECTS THE GUT
Normally, your large bowel absorbs most of the water from the leftover waste of
digestion and creates solid poo. But when the colon is affected by Microscopic
Colitis, it can’t absorb as much liquid from the waste. This can lead to an
imbalance of certain chemicals in the gut and mean that even more uid builds
up, producing a large volume of watery poo (diarrhoea).
SYMPTOMS OF MICROSCOPIC COLITIS
The main symptom of Microscopic Colitis is ongoing watery diarrhoea. This is
where you pass watery or loose poo more than three times a day for longer than
four weeks. For some people this can be as many as fteen times during the day
and night. It may begin suddenly or gradually, can happen at any time and may be
every time you go to the toilet, or only now and then.
The diarrhoea may:
• be sudden – you may not always reach the toilet in time
• be explosive - this is when your rectum has more watery poo and gas than it can
hold and it expels the poo with lots of force, often loudly
• happen several times a day and at night.
There usually isn’t any blood in the poo.
My symptoms include explosive
diarrhoea, stomach cramps and
tiredness. I’ve also lost a lot of
weight.
Lyn, age 60
living with Microscopic Colitis
MICROSCOPIC COLITIS
3
Crohn’s & Colitis UK | www.crohnsandcolitis.org.uk
Other symptoms can include:
• pain in the tummy area – which may be cramping or dull
• fatigue or extreme tiredness, this may be caused by getting up at night to go to
the toilet, but many people experience this even if they sleep through the night
• joint pain
• bloating and wind.
Living with symptoms
These symptoms can have a real impact on life. The uctuating nature can mean
some days aren’t good and you can feel that you no longer know your own body.
This can make going out with friends, work and planning activities really difcult.
Coping with these symptoms may make you feel isolated and low.
Our information on Fatigue, Joints, Bloating and Wind, and Managing Bowel
Incontinence can help you nd ways to manage these symptoms.
CAUSES OF MICROSCOPIC COLITIS
We don’t know yet what causes Microscopic Colitis. It’s thought that a combination
of factors trigger the body’s immune system to attack healthy cells in the lining of
the colon.
These include:
• Damage to the lining of the gut – this may be by caused by viruses, bacteria or
certain medicines.
• Genes a person has inherited.
• Other factors such as smoking, age and gender.
WHO GETS MICROSCOPIC COLITIS
You are more likely to get Microscopic Colitis if you:
• Are over 50 years old. Most people get Microscopic Colitis when they are aged
between 50 and 60. But 1 in 4 are under 25 and children have also been
diagnosed with the condition.
• Are female.
• Have an autoimmune condition - see below.
• Smoke cigarettes.
• Use certain medicines - see the list in the section Treatments for Microscopic
Colitis.
At least 1 in 1000 people are thought to have Microscopic Colitis in the UK, but
the real number could be a lot higher because it’s often underreported and
misdiagnosed. It’s less well known by both health professionals and the
general public which may mean many people with Microscopic Colitis are coping
in silence.
OTHER CONDITIONS ASSOCIATED WITH MICROSCOPIC COLITIS
Autoimmune conditions
Around 4 in 10 people with Microscopic Colitis also have a condition caused by
the immune system attacking other parts of the body (autoimmune condition).
These include:
• Type 1 diabetes
• thyroid disease
• coeliac disease
• rheumatoid arthritis.
Nobody told me some of the
things I might experience, like
fatigue or joint aches.
Helen, age 63
living with Microscopic Colitis
MICROSCOPIC COLITIS
4
Crohn’s & Colitis UK | www.crohnsandcolitis.org.uk
Bile acid malabsorption (BAM)
Around 4 out of 10 people with microscopic colitis also have BAM. Bile salts help
you to digest fats. When you eat a meal, especially with fat in it, these bile salts
are released from your liver and gall bladder into the upper part of your gut. They
help to digest the food as it travels through your small bowel. When the bile salts
reach the far end of this, they are mostly absorbed back into your body and return
to your liver in the bloodstream.
Bile acid malabsorption happens when the gut can’t direct bile acid back to the
liver. It’s thought that this irritates the lining of the colon and means that your body
doesn’t absorb water properly. This means you produce large amounts of watery
poo. Find out more in Diarrhoea and Constipation.
DIAGNOSIS
History of your symptoms
Your doctor will take a careful history of all your symptoms as some can be similar
to other conditions such as Irritable Bowel Syndrome (IBS).
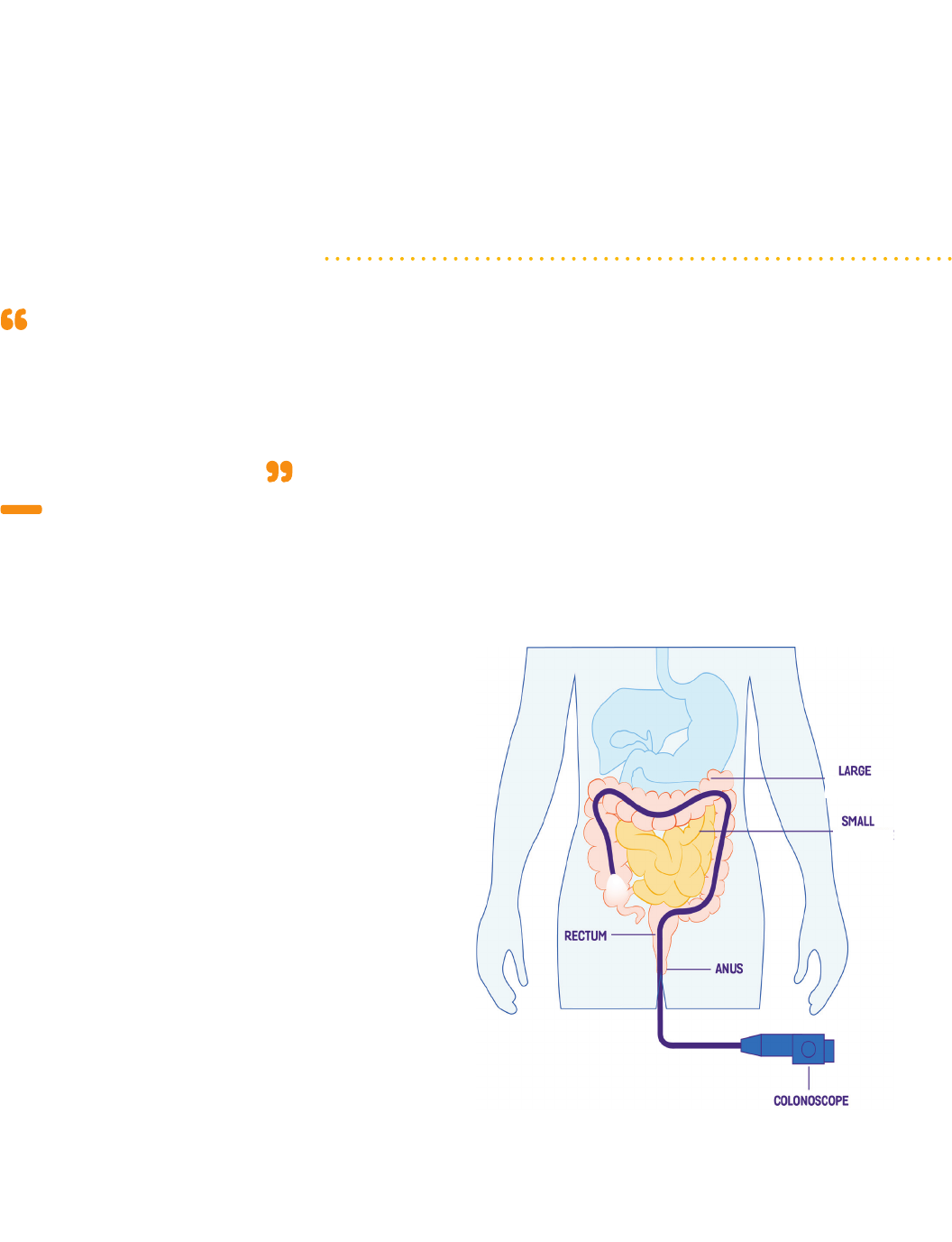
Colonoscopy with biopsy
In Microscopic Colitis, changes in the gut can only be seen under the microscope.
So, to diagnose the condition a small tissue sample (biopsy) is taken from the
colon when you have a colonoscopy. This is then looked at under a microscope.
In a colonoscopy, a long exible tube (about the thickness of your little nger)
with a bright light and camera at its tip is inserted through your anus. This allows
the doctor to have a look at the lining of your colon and painlessly remove small
pieces of tissue to look at under a microscope. A few samples are usually taken
from different parts of the colon.
A COLONOSCOPY
The doctor won’t be able to see any visible signs of inammation when they look
at your colon and rectum. This is different from Crohn’s or Ulcerative Colitis when
inammation or ulcers can be seen. Find out more in Tests and Investigations.
I was diagnosed by a biopsy
taken during a colonoscopy. This
followed 6 months of unexplained
weight loss, persistent frequent
diarrhoea and abdominal pain.
Michaela, age 54
living with Microscopic Colitis
bowel
bowel
MICROSCOPIC COLITIS
5
Crohn’s & Colitis UK | www.crohnsandcolitis.org.uk
Other tests you may have
You may have a test for bile acid malabsorption. This is usually carried out in
the Nuclear Medicine outpatient department of the hospital. You’ll be given a
small capsule of a synthetic bile salts to swallow which contains a small amount
of harmless radioactive material known as SeHCAT. You’ll then have a scan and
another one a week later. These will measure the absorption of the radioactive bile
salts. Find out more about bile acid diarrhoea in our information on Diarrhoea and
Constipation.
Delay in getting a diagnosis
It may take some time to get a diagnosis of Microscopic Colitis, and this can be
frustrating.
This may be because:
• A poo test (faecal calprotectin) isn’t usually helpful – this nds evidence of
inammation in the gut, but with Microscopic Colitis levels are often quite low.
• Your colon and rectum will look normal at colonoscopy - it is vital to take
biopsies to nd Microscopic Colitis.
• Symptoms may be similar other conditions such as Irritable Bowel Syndrome
(IBS) or coeliac disease which doctors may be more familiar with,
TREATMENTS FOR MICROSCOPIC COLITIS
Before you’re offered any treatment for Microscopic Colitis your doctor will review
the medicines you already take for other conditions.
Medicines that may trigger Microscopic Colitis include:
• non-steroidal anti-inammatory drugs (NSAIDs) such as ibuprofen, diclofenac
• some proton pump inhibitors (PPIs) such as omeprazole and lansoprazole used
to reduce stomach acid
• selective serotonin reuptake inhibitors (SSRIs) used to treat depression
• asprin
• acarbose for diabetes,
• ranitidine for indigestion and heart burn
• ticlopidine for blood conditions
• statins for cholesterol control.
Many of these medicines can also cause diarrhoea as a side effect. But if you are
taking any of these do not stop taking them until you’ve talked to your doctor.
Lifestyle changes
Cutting down alcohol and caffeine can be helpful in reducing diarrhoea. It’s often
useful to keep a record of when you stop or cut down and how your symptoms
change, such as in the food diary in Food.
•Try cutting down on caffeine – drink decaffeinated tea, coffee, soft drinks or
water and reduce the amount of chocolate you eat.
•Cut down alcohol – drinking less has been shown to help symptoms.
•Stop smoking - smoking increases the risk of Microscopic Colitis, and people
who smoke have symptoms which are worse and less likely to get better with
treatment. Your GP practice can offer support with stopping smoking.
It’s been hard to get a diagnosis
and treatment. Even after that
Microscopic Colitis is still not
considered to be as serious as
other conditons.
Lyn, age 60
living with Microscopic Colitis
Food triggers often change. I can
eat something perfectly well one
month and not the next.
Michaela,
age 54
living with Microscopic Colitis

MICROSCOPIC COLITIS
6
Crohn’s & Colitis UK | www.crohnsandcolitis.org.uk
Medicines
There may be several options for treatment depending the severity of the
symptoms you have.
•Loperamide
If you have mild Microscopic Colitis, medicines to stop diarrhoea, such as
loperamide, can be effective. These slow down muscle contractions of the
gut which makes food move through more slowly and allows more water to be
absorbed. Poo becomes rmer and less urgent. They can also help to control
symptoms whilst other medications take time to work. Find out more in our
information on Diarrhoea and Constipation.
•Bile acid sequestrants
These include colestyramine, colestipol or colesevelam. If Microscopic Colitis
is related to bile acid malabsorption (BAM), or you continue to have diarrhoea
despite other treatment, you may be offered this type of medicine. These bind to
the bile acids in your gut and help to improve symptoms of diarrhoea. It has been
suggested that this may be effective even where BAM isn’t present.
•Budesonide
This steroid has been found to be an effective treatment if you have moderate to
severe Microscopic Colitis. Around 8 out of 10 people have been shown to improve
when taking this medicine and there are usually few side effects.
The normal dose is 9mg of budesonide a day for 6 to 8 weeks. You may also
be offered loperamide to control the diarrhoea whilst the budesonide gets your
condition under control. Your symptoms may start to get better within one or two
days but for some people it can take around three and six weeks.
Over half of people on budesonide nd their symptoms come back when the
treatment stops. If this happens to you a lower dose may be tried, and this could
be continued for up to a year. As with all steroids this isn’t usually a long-term
option.
Most people get better with these approaches but if they don’t work for you other
treatments may be tried
•Biologic Medicines.
Iniximab and adalimumab have been shown in small studies to improve
symptoms for some people where budesonide hasn’t been effective. Small studies
also suggest that vedolizumab could be helpful. These medicines are taken by
infusion or injection and you can nd out more in our information on Biologic
Medicines.
•Immunosuppressants.
Azathioprine and mercaptopurine have been shown to be effective for some
people where budesonide hasn’t worked. Find out more in Azathioprine and
Mercaptopurine.
Surgery
Surgery is very rarely needed, but for the few people where other approaches
haven’t been successful this can be an option. You can nd out more about
possible operations in Surgery for Ulcerative Colitis.
Don’t give up. Find out about
Microscpic Colitis yourself. Your
GP is unlikely to know the answer
to all your questions so you can
go with the information and ask
for what you’d like help with.
Jaqui, age 35
living with Microscopic Colitis
MICROSCOPIC COLITIS
7
Crohn’s & Colitis UK | www.crohnsandcolitis.org.uk
MICROSCOPIC COLITIS AND RISK OF COLON CANCER
Microscopic Colitis does NOT make you any more likely to get colon cancer than
the general population.
MAKING CHANGES TO YOUR DIET
Diet with Microscopic Colitis is different for everyone. There isn’t evidence that
specic foods affect some people with Microscopic Colitis but you may nd that
some foods are a trigger for you. Fatty, spicy and high bre foods make some
people feel worse, but everyone is different, Many people ask:
•Should I avoid gluten? - People with Microscopic Colitis are more than 50 times
more likely than the general population to have coeliac disease. This means you’re
not able to digest a type of protein called gluten, which is found in wheat, barley
and rye. To nd out if you need to avoid gluten, your doctor will do a blood test to
check for this. If your blood test is positive, you may also have an upper
Gastrointestinal endoscopy to conrm. Find out more in Food and Tests and
Investigations.
•Should I avoid dairy products? – If your diarrhoea is worse after eating dairy,
you may have trouble digesting lactose - the type of sugar found mainly in milk,
cheese and other dairy products. Keeping a food diary to see how you feel can
help you to nd out if this is the case for you – try the one in Food. Sometimes a
simple breath test is used to nd out if you’re lactose intolerant.
Talk to your doctor or dietitian before making any major changes to your diet. They
can help you plan how to avoid dairy products or gluten while still getting the
nutrients you need.
WHO TO TALK TO IF YOU’RE WORRIED
Our Helpline takes many calls from people with Microscopic Colitis so you’re not
alone. We can’t advise but it may help to talk through your worries. Your doctor will
support you and you should ask for support from an IBD nurse-led service.
An IBD nurse can offer support and advice about treatment options, daily life with
Microscopic Colitis and help you to live well with IBD. But NHS support services
vary - some areas still don’t have an IBD nurse, whilst others have limited
resources and may not be able to support you if you have Microscopic Colitis.
Find out if your hospital has an IBD nurse at crohnsandcolitis.org.uk/ibdnurse
After many years of
experimenting, I’ve found dairy
products seem to trigger my
symptoms, so I’ve replaced milk
with soya or almond milk instead.
Lyn, age 60
living with Microscopic Colitis

MICROSCOPIC COLITIS
8
Crohn’s & Colitis UK | www.crohnsandcolitis.org.uk
HELP AND SUPPORT FROM CROHN’S & COLITIS UK
We’re here for you whenever you need us. Our award-winning publications on
Crohn’s and Colitis have the information you need to help you manage your
condition. We have information on a wide range of topics, from individual
medicines to coping with symptoms and concerns about relationships, school and
employment. We’ll help you nd answers, access support and take control.
All publications are available to download from our website
crohnsandcolitis.org.uk/publications
The It Takes Guts Talking Toolkit is an interactive tool with all the information,
talking tips and resources you’ll need to feel condent to start your conversation
about Microscopic Colitis. There are lots of personalised options based on who you
want to talk to and what your main worries are
www.ittakesguts.org.uk/talking-toolkit.
Helpline
Our Helpline is a condential service providing information and support to anyone
affected by Crohn’s, Ulcerative Colitis or Microscopic Colitis.
Our team can:
• help you understand more about Crohn’s and Colitis diagnosis and treatment
options
• provide information to help you to live well with your condition
• help you understand and access disability benets
• put you in touch with a trained support volunteer who has personal experience
of Crohn’s or Colitis.
Call us on 0300 222 5700 or email [email protected]
See our website for LiveChat: crohnsandcolitis.org.uk/livechat
Crohn’s & Colitis UK Forum
This closed-group community on Facebook is for everyone affected by Crohn’s
or Colitis. You can share your experiences and receive support from others at:
facebook.com/groups/CCUKforum
Crohn’s & Colitis UK Local Networks
Our Local Networks of volunteers across the UK organise events and provide
opportunities to get to know other people in an informal setting, as well as to
get involved with educational, awareness-raising and fundraising activities. Visit
crohnsandcolitis.org.uk/local-network to nd your nearest network.
Help with toilet access
If you become a member of Crohn’s & Colitis UK, you will get benets including
a Can’t Wait Card and a RADAR key. This card shows that you have a medical
condition, and combined with the RADAR key will help when you need urgent
access to the toilet when you are out and about. See our website for further
information: crohnsandcolitis.org.uk/membership or call the membership team
on 01727 734465.
OTHER ORGANISATIONS
Coeliac UK
coeliac.org.uk
0333 332 2033
Crohn’s & Colitis UK publications are research-based and produced in
consultation with patients, medical advisers and other health or associated
professionals. They are prepared as general information on a subject and
are not intended to replace specic advice from your own doctor or any
other professional. Crohn’s & Colitis UK does not endorse or recommend
any products mentioned.
Crohn’s & Colitis UK follows the principles of the Information Standard
scheme for Health and Care information producers. For more information
see
crohnsandcolitis.org.uk and the Information Standard website:
www.england.nhs.uk/tis.
We hope that you have found this leaet helpful and relevant. If you would
like more information about the sources of evidence on which it is based,
or details of any conicts of interest, or if you have any comments or
suggestions for improvements, please email the Publications Team at
[email protected]. You can also write to us at Crohn’s
& Colitis UK, 1 Bishops Square, Hateld, Herts, AL10 9NE or contact us
through the Helpline: 0300 222 5700.
ABOUT CROHN’S & COLITIS UK
We are Crohn’s & Colitis UK, a national charity ghting for improved lives
today – and a world free from Crohn’s and Colitis tomorrow. To improve
diagnosis and treatment, and to fund research into a cure; to raise
awareness and to give people hope, comfort and condence to live freer,
fuller lives. We’re here for everyone affected by Crohn’s and Colitis.
This publication is available for free thanks to the generosity of our
supporters and members. Find out how you can join the ght against Crohn’s
and Colitis: call 01727 734465 or visit crohnsandcolitis.org.uk.
/crohnsandcolitisuk
@CrohnsColitisUK
@crohnsandcolitisUK
Follow us
Crohn’s and Colitis UK is the working name for the National Association for Colitis and Crohn’s Disease. Charity registered in England and Wales Number 1117148,
Scotland Number SC038632. A company limited by guarantee in England: Company number 5973370.
1 Bishops Square|Hatfield |Herts|AL10 9NE|0300 222 5700 |[email protected]
© Crohn’s & Colitis UK 2019
Microscopic Colitis
Edition 5
Last review: Nov 2019
Next planned review: 2022
